April 16, 2024
Nestled in the foothills of the Cascade Mountains and surrounded by open meadows, lakes, and rivers, La Pine Community Health Center (La Pine CHC) has been a lifeline for residents of Central Oregon since 2009. As an award-winning federally qualified health center and patient-centered primary care home with a focus on Medicaid and low-income patients, especially older adults and rural communities, La Pine CHC is committed to caring for community members facing financial challenges and offers primary care, mental health, and dental services regardless of their ability to pay.
“Our outreach team is very involved with making sure patients can get to and from appointments,” said Erin Trapp, CEO at La Pine CHC. “Anything we can do that’s outside of the box, that’s creative, that may improve that access (to care), we definitely will try it.”
So when the opportunity arose to partner with OCHIN on a pilot project designed to help expand specialty health care options for rural communities like theirs, they seized it.
“If it works for us, great, but if we can figure out a solution that’s going to help 40 other clinics, then … we did something that’s a greater good,” Trapp said. “We were able to identify how this could really have a great impact.”
Understanding the importance of connected specialty care
Specialty care refers to medical services delivered by health care providers who have training and expertise in a particular area of medicine, such as cardiology or neurology. Access to specialty care is essential for patients with complex medical conditions to achieve their full health potential, prevent complications, and reduce emergency room visits by ensuring they receive the most suitable and effective treatment tailored to their specific needs.
Specialty care providers are able to stay current on the latest clinical best practices in their area of focus. They often have access to cutting-edge advances in medical technology, enabling them to offer specialized diagnoses and treatments that may not be accessible through primary care.
“I manage a lot of stuff as a primary (care provider)—and I think all primaries do—but at some point, we’re kind of the jack of all trades. There’s a limit to what I can do, and there’s just some stuff that I don’t know,” said Sarah Sperry, physician assistant at La Pine CHC. “The next best step is to send you to the specialist.”
However, OCHIN network data reflects local, regional, and national trends showing limited access to specialty care and extended wait times for specialists. These factors contribute to persistent health care gaps in rural and underserved communities.
The pilot project aimed to address these gaps and ensure access to specialty care. Its goals included driving measurable clinical efficiencies, reducing wait times, and improving care coordination while seamlessly integrating specialty care into the clinician workflow, including electronic health records.
Facing unique challenges
Rural and medically underserved communities, such as La Pine, face unique challenges and barriers to accessing specialty care, including long distances, provider shortages, and transportation issues for patients.
Moreover, the average wait time to see a specialist has increased to 58 days, according to a recent OCHIN network analysis. Significantly delayed referrals had only a 40% likelihood of being completed. Due to ongoing clinician shortages, an aging population, and systemic barriers that disproportionately affect rural communities, these wait times are expected to continue rising, compromising patient health and increasing costs to the system.
“Sometimes you make a referral, and it can take three to four weeks to get the patient in to see a specialist, and then you have to wait on a report,” Trapp said. “So that whole closed-loop system can be very delayed or sometimes nonexistent if the patient misses an appointment and you don't know they missed an appointment. There are a lot of things that can impact their care plan.”
Patients’ living environment and location often significantly affect their ability to heal appropriately, Trapp said. For example, “if someone needs frequent (wound) dressing changes, but … they’re homeless, and maybe they have to walk to and from their appointments and it’s the middle of winter, and they already have diabetic ulcers on their feet … sometimes it goes back to being able to access something close to them and have the services readily available.”
But a shortage of specialist providers means that often specialists only come to town one or two days a month, if that, Sperry said. “I don’t have a kidney doctor that’s out here, or a hematologist, or an oncologist.”
Many patients are also struggling with multiple chronic health issues. “I have a specific patient … that has diabetes and congestive heart failure … and he has to stop taking specific medications just to even get into town,” Sperry said. “And so every time he does that, there’s an increase in pain, an increase in stress on the heart … problems with medical aspects that occur with the distance to care.”
Most La Pine CHC patients live at least 30 miles away from the nearest specialist, lack adequate access to broadband internet, and live at or below the federal poverty level. Some are unable to afford the time off work or the cost of gas, while others lack personal transportation and rely on friends or family for a ride. Often, patients cancel far-away specialty appointments due to snow or inclement weather.
“Just driving back and forth is really hard for these patients, and so if we can get a quick answer from a specialist as to whether or not they think they need to make that drive in or not is huge,” said Shawnacy Herron, director of nursing at La Pine CHC.
Expanding innovative access for rural communities
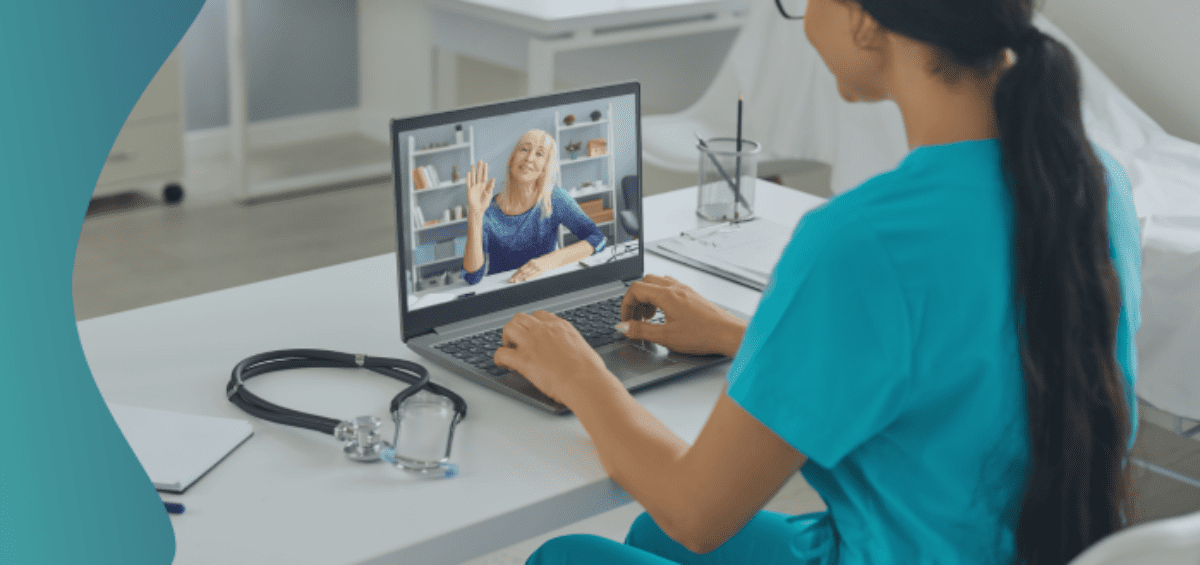
To address these challenges, La Pine CHC partnered with OCHIN and Dermatology Health Specialists on a pilot project to examine the effectiveness of dermatology eConsults in reducing follow-up time for patients. Supported by funding from the Central Oregon Health Quality Alliance, the project developed, tested, and implemented a new process in the OCHIN Epic EHR system that supports a virtual clinical referral workflow. This workflow was then used by primary care providers (PCP) to consult with a remotely located specialist for dermatological conditions in the patients they serve.
The project successfully created a reimbursable, electronic process in OCHIN Epic, which included the ability for a PCP to send digital images along with a related medical history and supporting documentation to a dermatologist. This process allowed PCPs to request and receive consultation with a specialist before referring a patient for an in-person visit, which reduced follow-up time for patients by an average of 45 days. Throughout the project, OCHIN was the “glue that held the whole process together,” Herron said.
“We were getting back responses pretty quickly, within a couple days to a week,” Sperry said. “It was definitely helpful in being able to respond pretty quickly to those patients.”
Most (59%) of eConsults were resolved without a traditional referral, and patients were able avoid an in-person visit to a dermatologist. “It was more of a wrap-around care model that was patient-centric. And I think that speaks volumes,” Trapp said.
Almost half of eConsults affected PCPs’ treatment plans, and PCPs reported increased confidence in their ability to correctly diagnose and treat common dermatologic conditions such as skin cancer. Sperry said that as a clinician, they gained valuable insights, receiving confirmation for some treatment plans while also discovering new ideas for future treatments.
“It's supporting our patients, but it’s also supporting our providers and giving them as many tools and resources available to help them better care for the patients.” Trapp said. “You can immediately start a care plan and get [patients] onto the road of better health."
The pilot project had significant financial benefits for the health center. The average payor savings per eConsult was $97, and patients saved an estimated $120 per avoided traditional referral from reduced travel and missed work expenses.
The project also helped La Pine CHC and OCHIN learn how to scale telehealth solutions to other specialties down the road and develop better communication and relationships between specialists and PCPs. “When I send someone to a specialist and I get a report back three months later, I may glance at it, but I’m not going to be as invested as if I had an engaged discussion or collaboration,” Sperry said.
“The thing that it taught us the most was that this is really good for really small communities … really, really rural communities. Because the cost for these individuals to travel for something that isn’t major can be huge,” Herron said.
Trapp agrees. “It’s about improving health care for anyone and everyone, no matter where you’re at.”