July 9, 2025
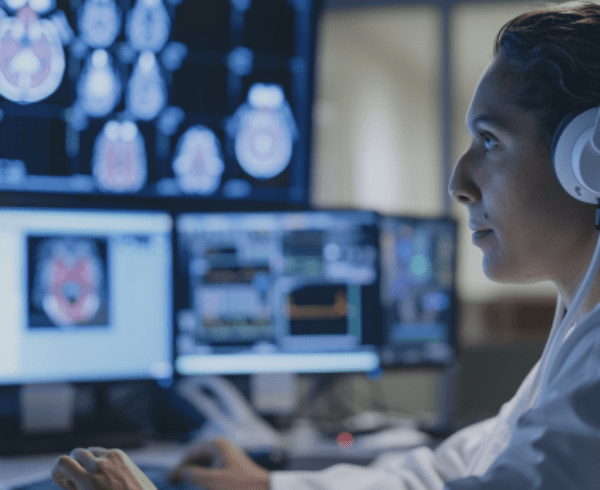
Contextual drivers of health, such as food, housing and transportation insecurity, can make it difficult for patients to follow their care plans. This often leads to poor health outcomes, especially for those with chronic conditions. Although many health care providers in community-based clinics recognize this and strive to adapt care plans to address these factors, little is known about how electronic health record (EHR) tools might assist providers in making these adaptations systematically.
To explore this, a team of researchers from OCHIN partnered with the Kaiser Permanente Center for Health Research and the University of California, San Francisco, to study whether such tools improve blood pressure (BP) and hemoglobin A1c (HbA1c) control and increase documentation of health drivers and related care plan adaptations in community clinics.
Rachel Gold, PhD, MPH, director of chronic disease, preventive health, and wellness research programs at OCHIN, answered a few questions about the Contextualized Care in Community Health Centers’ Electronic Health Records (COHERE) study, which concluded in May 2025.

What did you study and why?
Awareness of patients’ medical and non-medical health-related needs can prompt care teams to adjust care plans to reduce challenges to adherence. For example, adjustments might involve medication selection or modality of follow-up appointment scheduling. EHR tools could help care teams identify patients who might benefit from specific adjustments and document these changes. However, limited research evidence on such tools exists.
OCHIN conducted the nation’s first study on the impact of “social care decision support” tools to understand their usage and whether they improve health outcomes for patients with uncontrolled blood pressure or diabetes.
We collaborated with clinic partners to design a set of EHR tools. These tools notify care teams when a patient is due for screening for contextual drivers of health, allow quick documentation of reported drivers using standard codes, and facilitate documentation if a patient is not taking medications as prescribed due to cost. They also support documenting any care plan adjustments made in response to the patient’s contextual circumstances.
What did you learn?
We used data from 50 OCHIN clinics, six of which had the tools activated in their EHR. Tool use was optional, so we measured whether and how the tools were used and gathered feedback from clinic staff. We also assessed whether patients at clinics with the tools had improved blood pressure rates and diabetes control over the course of one year.
We found that blood pressure control was significantly better in clinics with the tools compared to those without, although the difference was small. No difference in diabetes control was found. Clinics with the tools documented the presence of contextual drivers more frequently overall and used standard codes significantly more often than clinics without the tools. However, the tools were rarely used for documenting care plan adjustments.
Clinic staff generally appreciated the tools that reminded them to screen for and document patients’ contextual drivers of health. However, they found the tools for documenting care plan adjustments to be less useful, as such adjustments were typically applied to most patients as a standard part of their practice.
Why does it matter?
Contextual drivers clearly impact the ability of people with chronic diseases to follow their medical care plans. It is important to find ways to help care teams minimize these impacts, especially in community clinics that serve populations facing such drivers. This study’s findings provide new evidence about whether EHR tools can support these efforts.
The trial results show that integrated EHR tools can help care teams ensure patients are screened, and that screening results are documented in a standardized way. This suggests there might be benefits to helping clinics access and use such tools.
The results also show a relationship between having these tools and blood pressure control rates, although the impact was small. It is not clear whether this improvement was caused by the tools supporting care plan adjustments, though some clinic staff liked having information on patient contextual drivers accessible in the EHR.
The low rates of tool use to document care changes might be because care teams did not find those tool elements useful or because teams need more support to integrate them into practice. More research is needed to understand how to make such tools more useful in different care settings.
Study findings add knowledge on the benefits of using technological tools to support team awareness of patient context and the challenges of using such tools to inform practice.
What was OCHIN’s role in this study?
All the clinics involved in this innovative study were members of the OCHIN network. A team of OCHIN scientists collaborated with the Kaiser Permanente Center for Health Research and the University of California, San Francisco.
This work is supported by the National Institute on Minority Health and Health Disparities under Award Number R01MD014886 (Gold, PI).
The research reported in this work was powered by PCORnet®. PCORnet has been developed with funding from the Patient-Centered Outcomes Research Institute® (PCORI®) and conducted with the Accelerating Data Value Across a National Community Health Center Network (ADVANCE) Clinical Research Network (CRN). ADVANCE is a Clinical Research Network in PCORnet® led by OCHIN in partnership with Health Choice Network, Fenway Health, University of Washington, and Oregon Health & Science University. ADVANCE’s participation in PCORnet® is funded through the PCORI Award RI-OCHIN-01-MC. This study has been approved and reviewed by the Kaiser Permanente Interregional Institutional Review Board.